Does Medicare Cover Cancer Treatment?
March 6, 2020Cancer is the second-most common cause of death in the US, right behind heart disease. A cancer diagnosis comes with a lot of uncertainty.
You might be unsure of how to tell your friends and family, or you might not know how you’ll pay for treatment.
After all, cancer treatment can be expensive. The average cost for cancer treatment is about $150,000, according to the American Association of Retired Persons (AARP).
The good news is that Medicare does cover cancer treatment, prescriptions, and screenings and might even cover genetic testing, depending on your plan.
Medicare Cancer Coverage: What you Need to Know

Cancer treatment usually involves a combination of treatments that can include chemotherapy, radiation, and surgery. Medicare plans can cover a lot of the costs associated with these treatment options.
What Cancer Treatment Does Medicare Cover?
In order for your treatment to be covered, your doctor must accept Medicare. Outpatient care (including intravenous chemotherapy, certain screenings, and outpatient radiation) falls under Part B.
You may have to pay a copayment, coinsurance and a deductible for each service.
Cancer treatment under Part A (hospital insurance) covers inpatient surgeries and hospital stays. Part A will also cover limited skilled nursing care and home health care services.
Original Medicare Coverage (Medicare Part A and Medicare Part B)
After you qualify at age 65, you’re enrolled in Medicare Part A and Part B, the Original Medicare. Medicare Part A covers inpatient hospital stays, which includes skilled nursing facility care, hospice care, and home health care.
Medicare Part B covers doctor visits, lab tests, and medical equipment and supplies.
Both Part A and Part B cover high-dose radiation treatments to shrink tumors and destroy cancer cells, but in different ways. Part A covers it for inpatients in hospitals.
Part B covers it for outpatients at independent (freestanding) clinics.
Medicare Advantage Plan Coverage
Medicare Advantage Plans are a health care plan offered by private health insurance companies that contract with Medicare and offer the full spectrum of Part A and Part B benefits.
Since these companies are legally expected to provide “equal or better” coverage than the original Medicare, a Medical Advantage Plan is sometimes also known as Medicare Part C.
Medicare Part D Coverage
Medicare Part D Coverage is an optional federal prescription drug plan for Medicare beneficiaries to pay for prescription drug coverage. You can get it as part of your original Medicare (Part A and Part B).
The annual premium for coverage in 2020 is $435, up from $415 last year.
Medicare Supplement Insurance (Medigap) Coverage
Medicare Supplement Insurance (Medigap) is worth buying to lower out-of-pocket costs if you want lower monthly premiums. Medigap plans cover many original Medicare costs, like copayments, coinsurance, or deductibles.
Does Medicare Cover Chemotherapy?
Medicare Part B covers chemotherapy drugs, radiation, and chemotherapy treatment for cancer patients in a doctor’s office, a clinic, a hospital, or even chemotherapy in a skilled nursing facility.
Medicare Part D plans cover cancer drugs like oral chemotherapy medications, anti-nausea drugs, and painkillers. Many people buy Medicare Supplement Plans (Medigap) plans to cover any dollar amount that Medicare does not cover.
Does Medicare Cover Immunotherapy for Cancer?
Immunotherapy is a cancer treatment that triggers your own immune system to fight off cancer cells. If immunotherapy is medically necessary, Medicare may cover many types of specialized treatments, for instance, immunotherapy for lung cancer.
Is CAR T-Cell Cancer Therapy Available to Medicare Beneficiaries?
The Centers for Medicare and Medicaid (CMS) approved Medicare coverage for FDA-approved Chimeric Antigen Receptor T-cell (CAR T-cell) to treat specific types of cancer, such as non-Hodgkin lymphoma and B-cell precursor acute lymphoblastic leukemia.
According to the Leukemia and Lymphoma Society (LLS), CAR T-cell therapy works by re-engineering a patient’s T-cells (disease-fighting cells), multiplying the cells, and re-introducing the “new” cells to the body.
Medicare Cancer Screening
Catching cancer in its early stages can make a huge difference in your treatment’s success.
That’s why Medicare offers coverage for preventive screenings for most cancers, including but not limited to:
- Breast cancer: Medicare will cover one annual mammogram, and one clinical breast exam (CBE) every two years for all women 40 and older who have an average risk of developing breast cancer. Women who are at a high risk of developing breast cancer can receive one CBE every year.
- Cervical cancer: Medicare pays for one pelvic exam and Pap test every two years. If you have a high risk of cancer, Medicare covers those tests once yearly.
- Colorectal cancer: Medicare covers certain colorectal cancer screenings looking for pre-cancer polyps for people 50 and older.
- Prostate cancer: Medicare covers one digital rectal exam (DRE) and one prostate-specific antigen (PSA) for men 50 and older. Medicare will cover 80% of the DRE and 100% of the PSA.
- Lung cancer: If you’re a smoker or have a long history of tobacco use, Medicare will cover low-dose CT scans for lung cancer.
Does Medicare Cover Wigs for Cancer Patients?
Hair loss is a common side effect of certain cancer treatments. Original Medicare and Medicare Supplements do not cover wigs. However, some Medicare Advantage plans may offer coverage for wigs.
Medicare Genetic Testing
Some people are at a higher genetic risk for cancer than others, meaning that they have specific gene mutations. Medicare will cover BRCA1 and BRCA2 genetic testing to find those mutations if you have a personal history of cancer.
Medicare also covers certain genetic tests for melanoma and colon cancer. Depending on where you live, that coverage extends to multigene testing if the initial test indicates multiple mutations.
Which Medicare Plan Is Best for Cancer Patients?
Americans spend $74 billion on cancer treatments each year, and Medicare covers almost half of that cost.
Medicare Part A, Part B, and Part D cover cancer treatment. Part A will cover up to 150 days stay in the hospital.
Part B will cover 80% of outpatient treatment, such as diagnostic imaging, injectable drugs, chemotherapy, radiation, and surgery. Part D will cover retail prescription drugs from a local pharmacy.
Medicare Special Enrollment Period and How to Qualify for Medicare Cancer Coverage
Open enrollment is a window of time from November 1, 2020, to December 15, 2020, to buy a healthcare insurance plan that is on the Federal Health Insurance Marketplace.
A cancer diagnosis means you qualify for the Medicare Special Enrollment Period (SEP). The SEP allows you to enroll in or change your plan as your treatment or other needs change.
Most people have to wait for the Annual Enrollment Period (AEP), which is from 10/15 to 12/7, to change coverage, but you can take advantage of the SEP.
Medicare Chronic Special Needs Plan (C-SNP)
If you are diagnosed with cancer, you may be eligible for a Chronic Special Needs Plan (C-SNP). C-SNPs are a form of Medicare Advantage designed specifically for those with certain chronic illnesses and conditions.
They go above and beyond the coverage that Original Medicare provides. For example, C-SNPs provide coverage for prescription drugs.
Your C-SNP will involve a network of providers that will communicate with each other about your treatment plan.
When to Enroll in a C-SNP
You can enroll in coverage as soon as you receive your cancer diagnosis, but you must get confirmation from your doctor that you have cancer. While you are allowed to enroll in a C-SNP before your doctor verifies the diagnosis, your doctor must verify the diagnosis before you can keep the coverage.
Does Medicare Cover Cancer Treatment After Age 76?
Medicare covers cancer treatment for those enrolled, including Medicare coverage over 70 years of age, but there may be a deductible or a copay. It also covers beneficiaries after they turn 76.
Can You Get Medicare Before 65 If You Have Cancer?
If you’re under 65 and get cancer, you are eligible for Medicare if you’ve been receiving Social Security Disability Insurance (SSDI) checks for 24 months or longer or if you have a diagnosis of End-Stage Renal Disease (ESRD).
How to Find an Oncology Doctor Who Takes Medicare
An oncology doctor, or oncologist, is a doctor who specializes in cancer treatment. Oncologists can have one of three different sub-specialties: medical, surgical, and radiation.
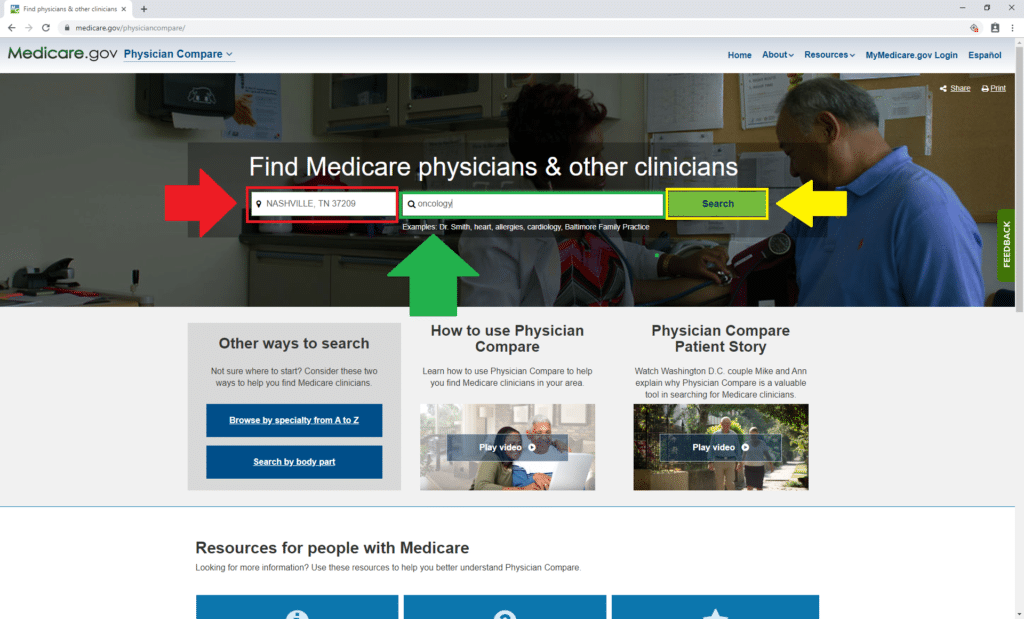
Medicare.gov has a tool for finding local oncologists who accept Medicare.
To get started, click here. First, enter your zip code beside the red arrow. We used 37209, because that’s the zip code for our corporate headquarters in Nashville, TN.
Then enter “oncology” in the box above the green arrow. Once you do that, click “Search” beside the yellow arrow.
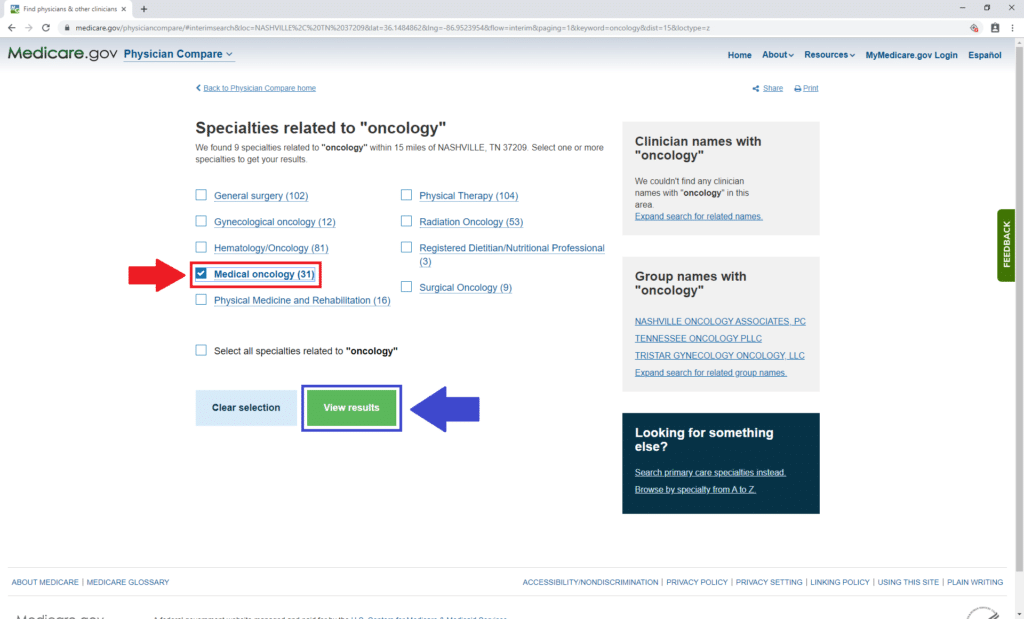
The next page will let you select what subspecialty you want your oncologist to have. You can select more than one, but for demonstration purposes, we only chose “Medical oncology” (below beside the red arrow).
Then click “View results” beside the blue arrow.
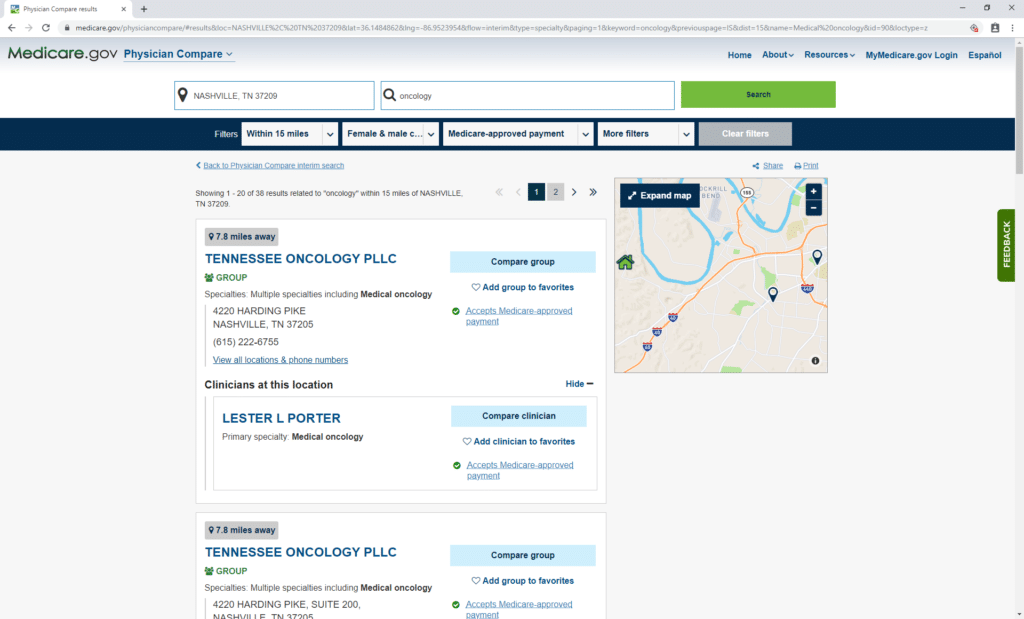
The next page features a list of medical oncologists complete with contact information. Call the doctors to get an idea of what services they provide and if they can treat you.
You may have to call multiple oncology doctors to find the right one.
We Can Help You Get Covered
A cancer diagnosis can be overwhelming, but the right medical coverage can help give you the chance to get the quality care you need.
If you have cancer and need to enroll in a C-SNP, we will assist you with finding the best insurance plan for you. Call us at (833)-567-3163 or contact us here today.

This post was originally published on April 19, 2019, and updated on March 6, 2020.

